The National Health Service (NHS) A Publicly Funded Model in the UK
The United Kingdom’s healthcare system is primarily delivered through the National Health Service (NHS), a widely recognized publicly funded model established on the principle of universal care. Financed predominantly through general taxation, the NHS ensures that the vast majority of services are free at the point of use for all legal residents of the UK [Source: NHS – How the NHS is funded]. This means that for consultations with a general practitioner, emergency care, and most hospital stays, patients typically do not incur direct costs. The overarching goal of this system is to provide comprehensive medical care to everyone, with access determined by clinical need rather than an individual’s ability to pay [Source: The King’s Fund – Key principles of the NHS].
This publicly funded approach fosters a sense of collective responsibility for health outcomes across society, aiming to remove financial barriers that might prevent individuals from seeking necessary medical attention. While the “free at point of use” principle is a cornerstone, it’s important to note certain nuances. For instance, prescription medications in England typically incur a standardized charge per item. However, an extensive list of exemptions ensures that vulnerable populations, including children, seniors (over 60), pregnant women, those with specific long-term medical conditions, and individuals on low incomes, are not burdened by these costs [Source: NHSBSA – Who can get free NHS prescriptions].
Despite its commitment to universal access, the NHS faces considerable challenges, particularly concerning waiting lists. Patients may experience delays for certain elective procedures, non-urgent specialist appointments, or diagnostic tests [Source: Nuffield Trust – NHS waiting times for referral to treatment]. These waiting times are often a consequence of high demand, resource constraints, and workforce shortages, which are ongoing issues for the system. Despite these challenges, the NHS remains a highly valued institution, deeply embedded in the UK’s social fabric, symbolizing a commitment to healthcare as a fundamental right.
The United States A Market Based Healthcare Landscape
In stark contrast to the UK, the United States operates a complex and largely market-based healthcare system, characterized by a dynamic mix of private and public insurance programs. The vast majority of Americans obtain health coverage through their employers, a legacy system where employers often subsidize a significant portion of insurance premiums [Source: KFF – Total Population with Health Coverage]. For those not covered by an employer, options include purchasing plans directly from private insurers or through state and federal marketplaces established under the Affordable Care Act (ACA).
Alongside private insurance, crucial public programs serve specific demographic groups. Medicare provides health coverage for individuals aged 65 and older, as well as some younger people with disabilities. Medicaid, on the other hand, offers a vital safety net, providing care for low-income families and individuals, though its eligibility rules and benefits can vary significantly by state [Source: Centers for Medicare & Medicaid Services (CMS) – What We Do]. This multi-payer framework results in a highly fragmented system where access to care, choice of providers, and financial obligations can differ dramatically based on an individual’s insurance plan.
One of the most defining characteristics of the US system is the potential for significant out-of-pocket costs for patients. These can include deductibles (the amount paid before insurance coverage kicks in), co-pays (a fixed amount paid for a service), and co-insurance (a percentage of the cost paid after the deductible is met). These costs vary widely based on the specific insurance plan and can accumulate rapidly, leading to substantial financial burdens for individuals and families [Source: Advisory Board – Understanding Out-of-Pocket Costs]. The financial implications can be severe, with medical debt being a significant issue for many Americans, even those with insurance.
The market-driven nature of US healthcare also contributes to its high expenditures. The United States consistently records some of the highest healthcare spending per capita globally, often without achieving superior health outcomes compared to other developed nations [Source: Health System Tracker – How does health spending in the U.S. compare to other countries?]. This elevated spending is attributed to various factors, including higher prices for drugs and services, administrative complexities, and the widespread use of advanced medical technology. Consequently, access to timely and appropriate care in the US can be heavily influenced by the extent and quality of one’s insurance coverage, leaving uninsured or underinsured individuals facing significant barriers to necessary medical services.
Comparing Philosophies Universal Access vs Market Competition
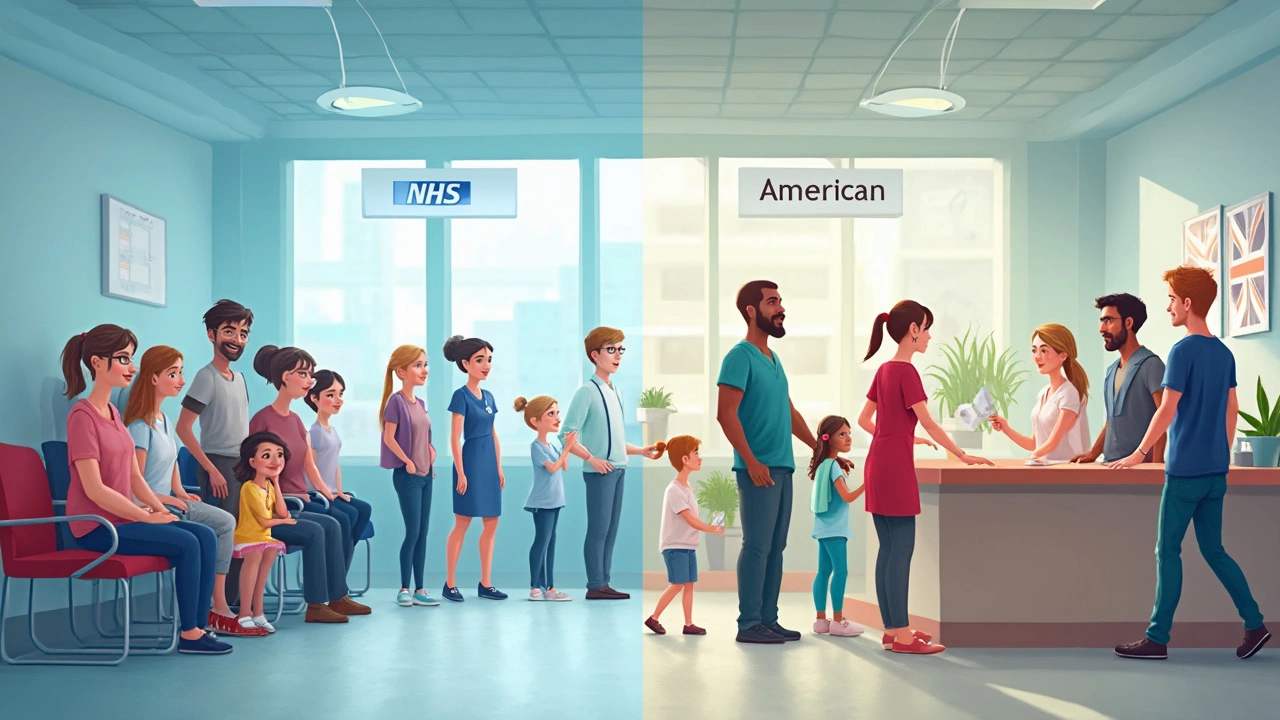
The divergent approaches of the UK and US healthcare systems reflect fundamentally different philosophies regarding the role of government, individual responsibility, and the provision of essential services. The NHS embodies the principle that healthcare is a universal right, a collective good to be provided equally to all citizens, regardless of their socioeconomic status. This approach prioritizes equity and financial protection, aiming to eliminate the fear of medical bankruptcy. While it ensures broad access, the trade-off can manifest as centralized control and, at times, reduced patient choice or longer waits for non-emergency treatments.
Conversely, the US system, with its market-based underpinnings, often emphasizes individual choice, innovation, and competition among providers. Proponents argue that this fosters higher quality care and quicker access for those who can afford premium plans. However, this comes at the cost of significant disparities in access and financial vulnerability for a large segment of the population. The emphasis on individual purchasing power means that a person’s health outcomes can be inextricably linked to their financial situation and the quality of their insurance.
These differences lead to distinct patient experiences. In the UK, a patient might experience peace of mind regarding medical costs but could face a waiting list for an elective knee surgery. In the US, a patient with comprehensive insurance might get that surgery quickly from a surgeon of their choice, but even then, they could still face a substantial bill due to deductibles or co-insurance. For an uninsured US patient, the same surgery could be financially ruinous or simply inaccessible.
Ultimately, both systems strive to provide effective medical care but navigate the complexities of resource allocation, access, and affordability through vastly different mechanisms. The ongoing debates in both nations highlight the persistent challenges of balancing universal access, cost containment, quality of care, and patient choice in modern healthcare.
Sources
- Advisory Board – Understanding Out-of-Pocket Costs: Deductibles, Coinsurance, and Copays
- Centers for Medicare & Medicaid Services (CMS) – What We Do
- Health System Tracker – How does health spending in the U.S. compare to other countries?
- KFF – Total Population with Health Coverage (Data by State)
- The King’s Fund – Key principles of the NHS
- NHS – How the NHS is funded
- NHSBSA – Who can get free NHS prescriptions
- Nuffield Trust – NHS waiting times for referral to treatment
Conclusion:
The UK’s NHS, funded through taxation, provides universal healthcare free at the point of use, prioritizing equity but often facing waiting time challenges. In contrast, the US system is market-based, relying on a mix of private insurance and government programs like Medicare and Medicaid, which can lead to high costs and unequal access. While the NHS views healthcare as a right, the US system treats it as a commodity, emphasizing choice and innovation but with greater financial risks for patients.